To the Editor:
We are very pleased to note Dr. Meldrum’s “Conceptions” piece (1), following our recent report (2), reaffirming our main conclusion that the current IVF outcome reporting system requires a major overhaul. Dr. Meldrum, furthermore, emphasizes other points raised in our article, including the need for ART reports to incorporate maternal and perinatal outcomes rather than just pregnancy rates in defining assisted reproductive technology (ART) success, to better align reports with patient interests (3). We also agree with basing outcome reports on the total reproductive potential (TRP) of each initiated in vitro fertilization (IVF) cycle, which includes the initial fresh cycle plus subsequent frozen transfers, a process feasible from the current Society for Assisted Reproductive Technology (SART) database (4).
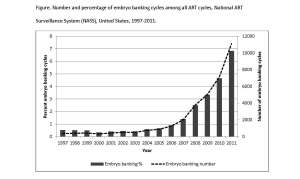
Dr. Meldrum’s main proposal of reporting outcome data on a per embryo transfer basis will, however, not solve the problem of outcome data manipulation in IVF, which our report brought into the open (2). In fact, reporting outcome data on a per embryo transfer basis may actually further exacerbate exclusion of poor prognosis patients who start cycles but, for various reasons (embryo banking with unsuccessful subsequent thaw, all embryos degenerate in extended day-5/6 culture, all embryos aneuploid after preimplantation genetic screening (PGS), etc.), never reach embryo transfer. Exactly these kinds of exclusions currently allow a small minority of reporting centers to disproportionately select out patients with low pregnancy potential and, thereby, to manipulate pregnancy rates in the centers’ favor (2). Read the rest of this entry »